Objective: Most infections with Enterobacteriaceae producing AmpC β-lactamase (AmpC)-, extended-spectrum β-lactamase (ESBL)-, and carbapenemase-producing bacteria, vancomycin-resistant Enterococcus as well as naturally resistant non-fermenting bacteria such as Pseudomonas aeruginosa, are related to a prior colonization of the gut microbiota. The objective of this study was to determine whether treatment with probiotics during an antibiotic treatment could prevent the colonization of the gut microbiota with multi-drug resistant bacteria.
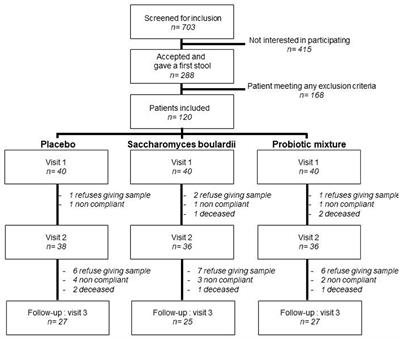
Method: In total, 120 patients treated for 10 days with amoxicillin-clavulanate antibiotics were included in a randomized, placebo-controlled, double-blinded trial, comparing the effects of a 30 days treatment with placebo Saccharomyces boulardii CNCM I-745® and a probiotic mixture containing Saccharomyces boulardii, Lactobacillus acidophilus NCFM, Lactobacillus paracasei Lpc-37, Bifidobacterium lactis Bl-04, and Bifidobacterium lactis Bi-07 (Bactiol duo®). Study treatment was initiated within 48 h of the antibiotic being initiated. Most of the patients included were elderly with a mean age of 78 years old with multiple comorbidities. Stools were collected at the time of inclusion in the trial, at the end of the antibiotic treatment, and the end of the study treatment. These were cultured on selective antibiotic media.
Results: Treatment with the probiotic mixture led to a significant decline in colonization with Pseudomonas after antibi otic treatment from 25 to 8.3% (p = 0.041). Colonization with AmpC-producing enterobacteria was transiently increased after the antibiotic treatment (p = 0.027) and declined after the probiotic intervention (p= 0.041). No significant changes were observed in the placebo and Saccharomyces groups. Up to 2 years after the trial, no infection with ESBL-producing bacteria was observed in the probiotic mixture group.
Conclusion: The association of Saccharomyces boulardii with specific strains of Lactobacillus and Bifidobacterium influences antibiotic treatment by counteracting the colonization of the colon microbiota with antibiotic-resistant pathogens.


Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου